
The PALS Bradycardia Algorithm is a systematic approach to treating slow heart rates in pediatric patients. This algorithm helps healthcare providers make quick, evidence-based decisions when children present with symptomatic bradycardia—a condition that can rapidly progress to cardiac arrest if not treated properly.
Bradycardia in children differs significantly from adults. While adults typically develop bradycardia due to heart disease, pediatric bradycardia often results from hypoxia, respiratory issues, or other underlying conditions. The PALS Bradycardia Algorithm addresses these unique aspects of pediatric emergency care.
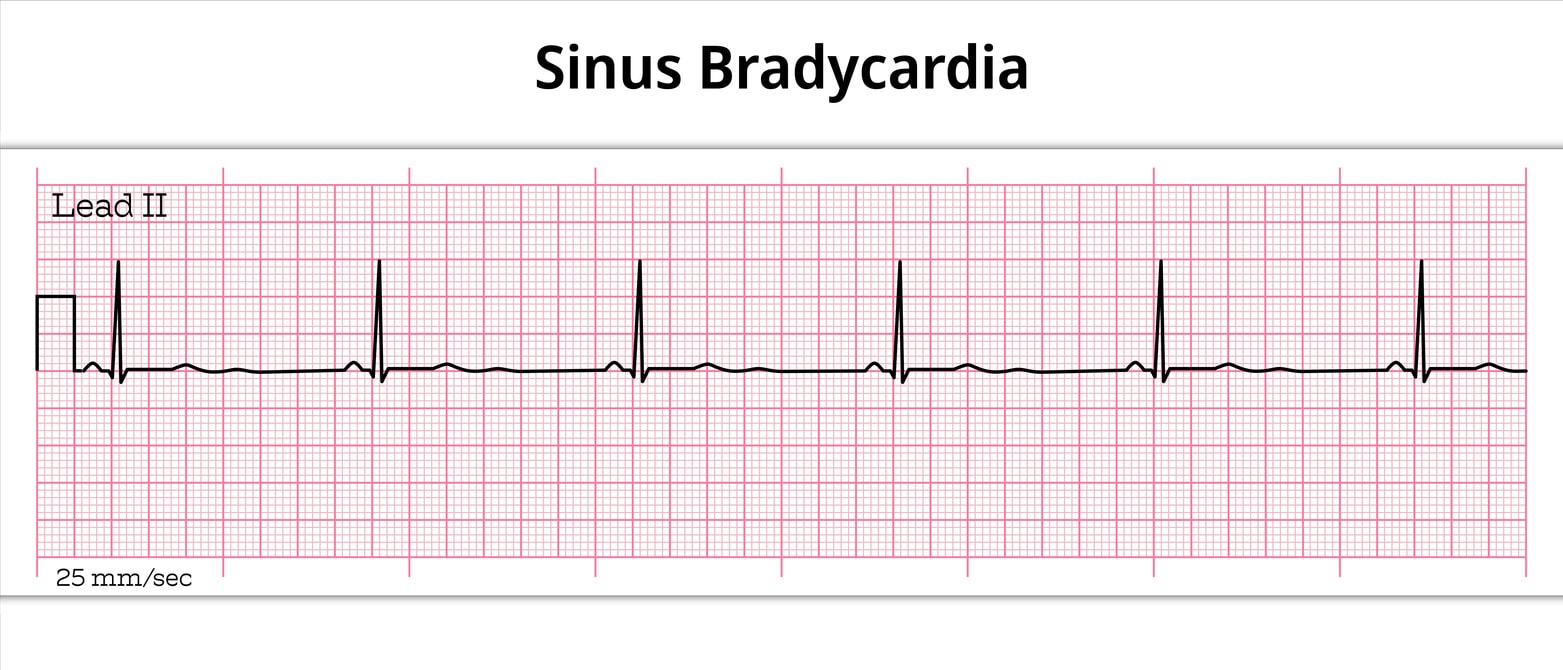
Bradycardia means “slow heart.” In children, normal heart rates vary significantly by age. Newborns typically have heart rates between 120-160 beats per minute, while adolescents may have rates as low as 60-100 beats per minute.
The key question isn’t just whether the heart rate is slow—it’s whether the slow rate is causing problems. Symptomatic bradycardia occurs when the heart rate is too slow to maintain adequate cardiac output for the child’s metabolic needs.
Common signs of symptomatic bradycardia include:
The algorithm begins with recognizing bradycardia that’s causing hemodynamic compromise. Look for heart rates below normal for age combined with signs of inadequate perfusion.
Check for these critical signs:
If the child has bradycardia but appears well-perfused and alert, continue monitoring rather than intervening aggressively.
Before moving to specific bradycardia treatments, ensure basic life support measures are in place. Most pediatric bradycardia results from hypoxia, making airway and breathing support crucial.
Provide high-flow oxygen and assist ventilation if needed. Establish vascular access—intraosseous access often works faster than IV access in emergency situations.
Consider reversible causes during this phase:
If the child remains symptomatic despite adequate oxygenation and ventilation, consider emergency interventions. The algorithm splits into two pathways based on the severity of symptoms.
For children with severe cardiopulmonary compromise, emergency transcutaneous pacing may be necessary. This includes children who are:
If pacing is not immediately available or ineffective, epinephrine becomes the drug of choice. The dosing differs from adult protocols:
IV/IO epinephrine dose: 0.01 mg/kg (0.1 mL/kg of 1:10,000 solution)
Maximum single dose: 1 mg
Epinephrine increases heart rate and contractility while improving blood pressure. Repeat every 3-5 minutes as needed.
Atropine may help in certain cases of bradycardia, particularly when increased vagal tone contributes to the slow heart rate. However, it’s less reliable in pediatric patients than in adults.
Atropine dose: 0.02 mg/kg IV/IO
Minimum dose: 0.1 mg
Maximum single dose: 0.5 mg
Atropine works by blocking vagal stimulation of the heart. It’s most effective in bradycardia caused by increased vagal tone rather than hypoxia or structural heart disease.
If initial treatments fail, prepare for more advanced interventions:
Transcutaneous pacing: Set rate 10-20% above intrinsic rate
Transvenous pacing: May be needed for persistent bradycardia
Expert consultation: Consider calling pediatric cardiology or intensive care
Understanding why children develop bradycardia helps guide treatment decisions. Unlike adults, children rarely develop bradycardia from primary heart disease.
Respiratory causes top the list:
Neurological causes include:
Metabolic causes encompass:
Toxic causes involve:
The PALS Bradycardia Algorithm differs from adult protocols in several important ways. These differences reflect the unique physiology of children and the different causes of bradycardia in pediatric patients.
Children have higher baseline heart rates and depend more heavily on heart rate to maintain cardiac output. They cannot increase stroke volume as effectively as adults, making heart rate maintenance crucial.
Drug dosing differs significantly. All medications are weight-based rather than fixed doses. This requires accurate weight estimation or measurement in emergency situations.
The approach to pacing also differs. Children may not tolerate transcutaneous pacing as well as adults, and the technique requires specific pediatric considerations for pad placement and energy settings.
Healthcare providers caring for children should maintain current PALS certification. The American Heart Association updates PALS guidelines regularly based on new research and clinical experience.
PALS training covers not just algorithms but also the critical thinking skills needed to adapt protocols to individual patients. Real pediatric emergencies rarely follow textbook presentations perfectly.
Mastering the PALS Bradycardia Algorithm requires hands-on practice and regular recertification. At Safety Training Seminars, we provide comprehensive PALS training that goes beyond memorizing algorithms. Our American Heart Association-certified instructors help healthcare providers develop the confidence and skills needed for real pediatric emergencies.
We offer PALS courses throughout California with convenient scheduling options. Our blended learning approach combines online coursework with hands-on skills practice, ensuring you’re prepared for actual clinical scenarios. With over 70 locations and same-day certification cards, we make it easy to maintain your credentials.
Our PALS training covers all critical algorithms, including bradycardia management, tachycardia treatment, and cardiac arrest protocols. We also provide continuing education credits for healthcare professionals who need them for license maintenance.
Ready to enhance your pediatric emergency skills? Contact Safety Training Seminars today to schedule your PALS certification or renewal. Our experienced team is available seven days a week to help you find the perfect class time and location.